Weekly Column: Health Care Flexibilities--Lessons Learned From The Pandemic
Guest column submitted by U.S. Senator Mike Crapo
Telehealth services have been especially useful during the COVID-19 pandemic. According to the Idaho Department of Insurance, telemedicine visits went from 200 appointments per month to 28,000 visits in April 2020 alone. We can use lessons-learned from the expansion of telehealth and other flexibilities to make sensible changes that can better enable Idahoans’ access to quality care going forward. Information on the impact of expanded telehealth on access, quality and cost helps guide permanent policy changes for the better.
As Ranking Member of the U.S. Senate Finance Committee, I have expressed interest in permanently extending health care flexibilities adopted during the pandemic with President Biden’s nominees for key health care positions who have come before the Committee. Republicans and Democrats often disagree on the best way to achieve shared health care goals. However, we have common ground on this issue. In May, the Committee held a hearing, planned jointly with Finance Committee Chairman Ron Wyden (D-Oregon), to discuss what we can learn from experiences with the health care flexibilities adopted during the pandemic to inform what changes should be made to improve health care access beyond the pandemic. We reviewed the waivers and flexibilities made available in the Medicare and Medicaid programs during the pandemic, with telehealth as a key topic. Health care providers, a health policy expert and the U.S. Government Accountability Office (GAO), which Congress tasked with monitoring the federal government’s pandemic response, provided insight to guide our evaluation.
The Centers for Medicare and Medicaid Services waived more than 200 payment rules during the pandemic in Medicare alone. The GAO reported, “Medicare telehealth waivers resulted in increased utilization of telehealth services, and provided beneficiaries access to services that would not have otherwise been available during the early days of the COVID-19 pandemic.” Reliance on telehealth increased in rural and urban areas alike, allowing patients to receive remote care from the safety of their home.
To ensure financial stability, providers have been paid at the same rate as if the service was furnished in-person. This has facilitated care that otherwise would be risky or unavailable, and patients have appreciated the convenience. It has reduced the frequency of missed appointments, and assisted provider investment in the infrastructure needed for remote care. This long period of expanded telehealth will help us understand the impact on quality of care and program costs. It serves as a robust test project on a scale few could have imagined.
Permanent changes based on lessons learned from the pandemic to modernize Medicare payment systems related to telehealth or through other care efficiencies lend to the pressing need to address Medicare’s financial struggles. Identifying smart reforms that make Medicare more efficient will be better for patients and better for taxpayers. Such changes alone will not put Medicare on a sustainable path, but they should be part of that broader conversation. Addressing Medicare solvency should also be a bipartisan issue, with time best spent determining how to shore up the current system instead of further stressing the cracks in the dam by expanding it to a broader population.
Finding the right path on these priority issues is important to all Idahoans and Americans. The GAO found that Medicare spent about $910 billon on health care services provided to about 62.8 million Medicare beneficiaries in 2020, while Medicaid covered an estimated 77 million people and spent an estimated $673 billion (total federal and state). I look forward to further seizing this bipartisan opportunity to take advantage of what the pandemic has taught us to ensure access to high-quality health care options for those in Idaho and across our country.
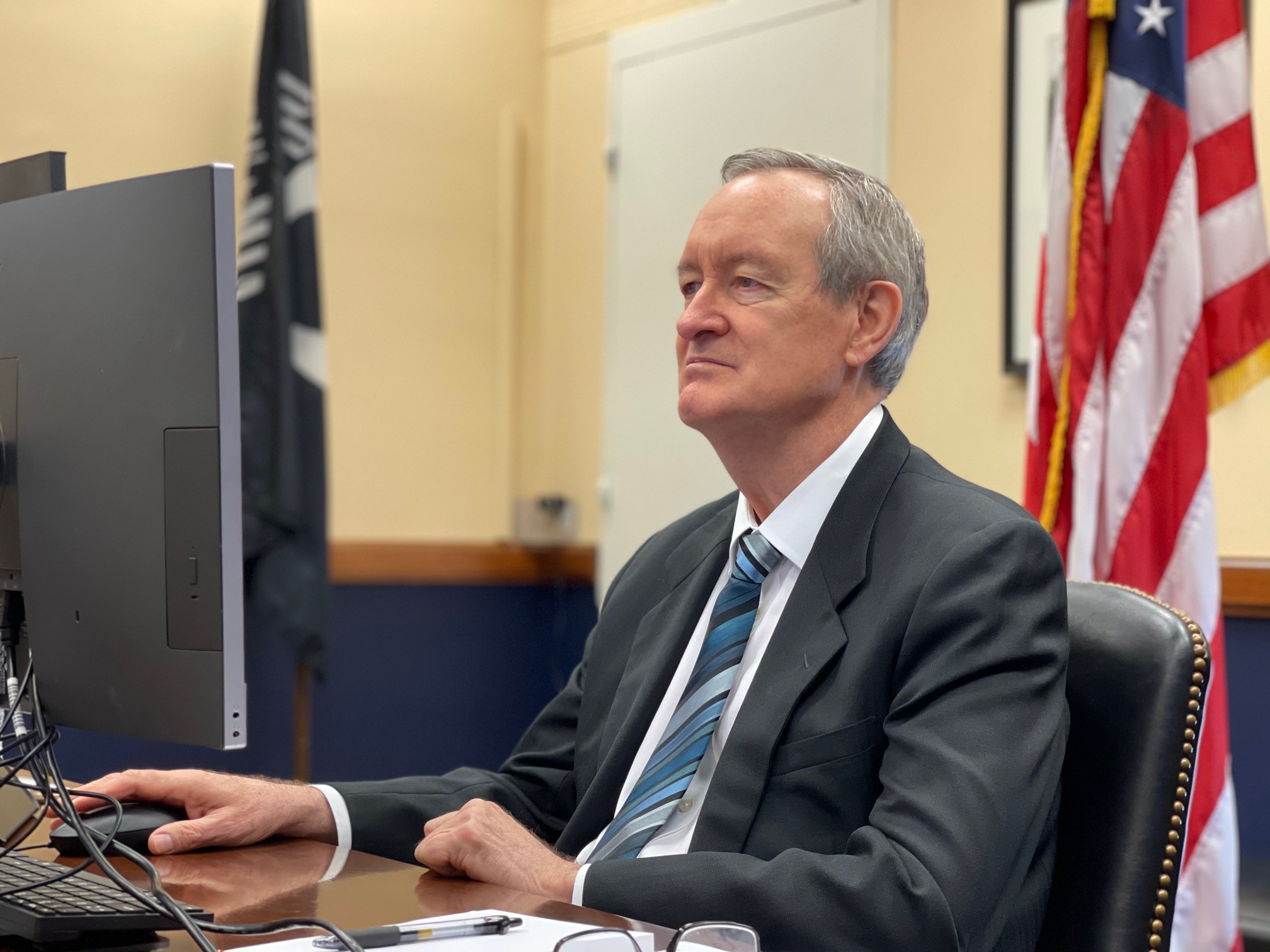
(Senator Crapo participating in May 19, 2021, Senate Finance Committee hearing, titled “COVID-19 Health Care Flexibilities: Perspectives, Experiences and Lessons Learned)
# # #
Word Count: 600
